Spider Veins Treatment in Hollywood, CA
Evidence-Based Care at Vein & Wound Center of LA
Spider veins (telangiectasias) are small red, blue, or purple vessels near the surface of the skin. They are most common on the thighs, calves, and ankles and may also appear on the face. While often considered cosmetic, this vein condition can sometimes reflect underlying venous reflux, making a specialist evaluation important.
At the Vein & Wound Center of LA in Koreatown, Dr. Christopher Kim provides medical assessment and minimally invasive treatment options tailored to each patient’s vein pattern and symptoms.
What Are Spider Veins?
Spider veins are tiny blood vessels that form web-like or starburst patterns. They often appear as:
- Fine red, blue, or purple lines
- Clusters resembling a “spider web”
- Veins most visible on the legs and sometimes the face
They are more common in women and may be influenced by age, pregnancy, genetic factors, and prolonged standing.
Symptoms of Spider Veins
• Mild itching or burning
• Localized tenderness
• Achiness after standing
• Sensitivity around dense clusters
• Cosmetic visibility
These symptoms can suggest a feeding reticular vein or nearby venous hypertension.
Risk Factors
Spider veins are more likely to develop in individuals with:
- Family history of venous issues
- Occupations that involve prolonged standing
- Pregnancy or hormonal shifts
- Previous leg trauma
- Age-related changes in the skin and vessel walls
- Prior vein treatments where feeder veins were not addressed
How Spider Veins Progress
Spider veins may remain unchanged for years, gradually multiply, spread into visible clusters, darken when pressure increases from deeper veins, or recur when underlying reflux is not treated. These patterns help determine whether cosmetic treatment alone is appropriate or if deeper evaluation is recommended.
Anatomy of Spider Veins — How and Why They Form
Spider veins develop within the dermis and superficial subcutaneous tissue just beneath the skin. These small dilated veins measure approximately 0.1–1 mm in diameter and are more visible because their walls are thin and lack the muscle layer found in deeper veins.
Skin and Vessel Layers Involved
• Epidermis: Protective outer layer without blood vessels
• Dermis: Contains venules where spider veins appear
• Subcutaneous tissue: Contains reticular veins and perforators that may act as feeders
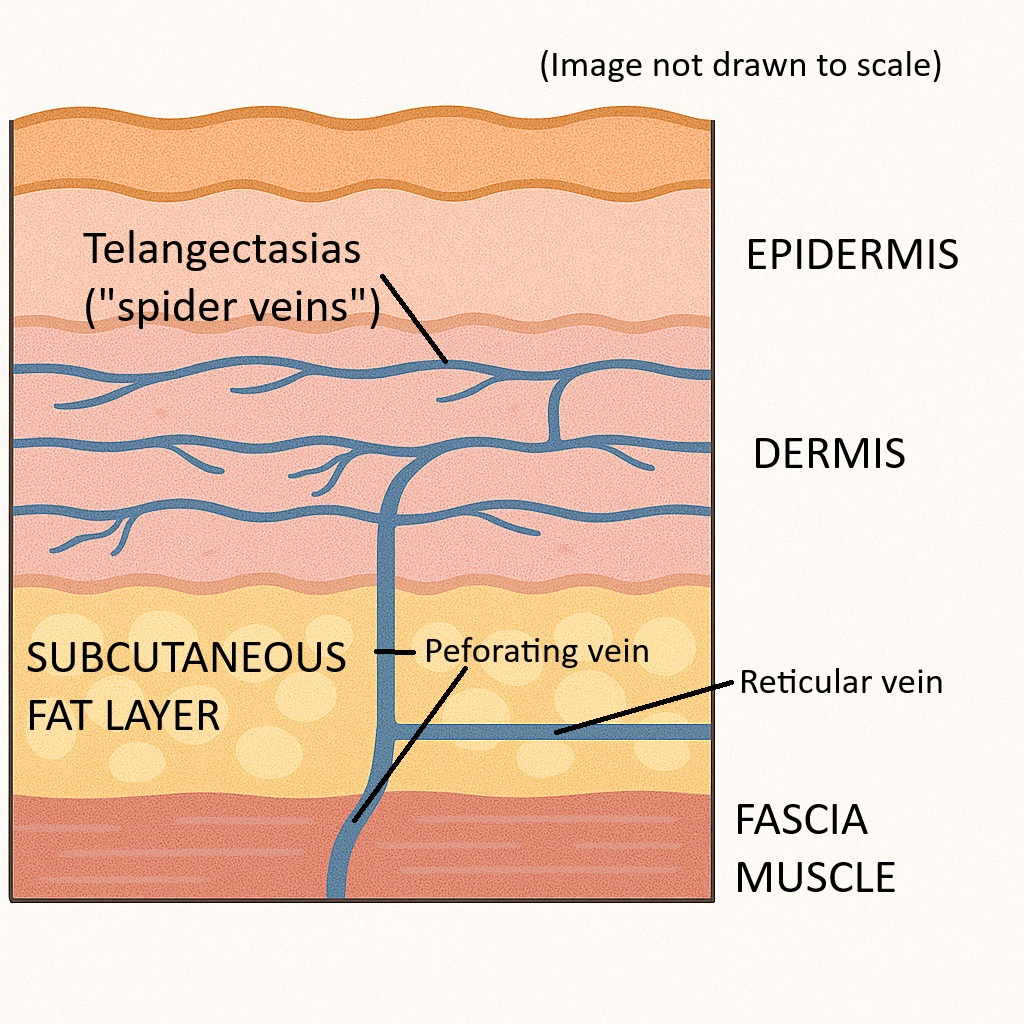
Why Spider Veins Form
• Dermal venules lose tone due to age, hormones, genetics, or pressure
• Vessel walls stretch easily
• Pressure from reticular or perforator veins can push blood toward the surface
• Estrogen and progesterone weaken vein walls
Feeder (Reticular) Veins
A slightly larger underlying vessel can feed a spider vein cluster. Failure to address the feeder (reticular) veins may lead to recurrence, matting, or partial clearing.
Pregnancy and Spider Veins
During pregnancy, increased blood volume, hormonal relaxation of vessel walls, and compression of pelvic veins raise pressure in the legs. Some spider veins fade postpartum, while others persist.
Spider veins form in the tiny surface veins just below the skin. When pressure builds—due to hormones, genetics, or underlying feeder veins—these veins stretch and become visible. Some clusters are purely cosmetic, while others have deeper sources that influence the durability of results.
What Spider Veins Are NOT
To avoid confusion, it’s helpful to distinguish spider veins from similar conditions:
• Varicose veins: Larger, rope-like bulging veins
• Bruising: Temporary discoloration that fades over days
• Cherry angiomas: Small bright-red raised bumps
• Normal blue veins: Healthy veins visible through thin skin
Treatment Options for Spider Veins in Los Angeles
We offer safe, evidence-based treatments performed in-office with no general anesthesia.
Non-Invasive Care
• Compression stockings
• Activity modification
• Leg movement and positional changes
These approaches may improve comfort but do not eliminate spider veins.
Minimally Invasive Procedures
• Liquid sclerotherapy: First-line treatment; closes surface veins
• Foam sclerotherapy: Ideal for larger clusters or feeder veins
• Long-pulsed 1064 nm Nd:YAG laser: Useful for very fine or facial veins
• Microphlebectomy: Removes or disrupts feeder veins when needed
Multiple sessions are often necessary, especially for dense or complex networks.
Why Duplex Ultrasound Matters
Some spider veins are isolated surface findings, while others are influenced by deeper venous patterns.
• Treating surface veins alone may lead to recurrence
• Duplex ultrasound (DUS) maps blood flow and identifies hidden reflux
• Clinical guidelines recommend DUS when symptoms or reticular veins suggest deeper involvement
• Ultrasound guidance during treatment can help locate feeder veins
• Spider veins may or may not be associated with Great Saphenous Vein (GSV) reflux
At Vein & Wound Center of LA, DUS is performed when indicated to address both appearance and underlying circulation.
Potential Complications of Spider Vein Treatment
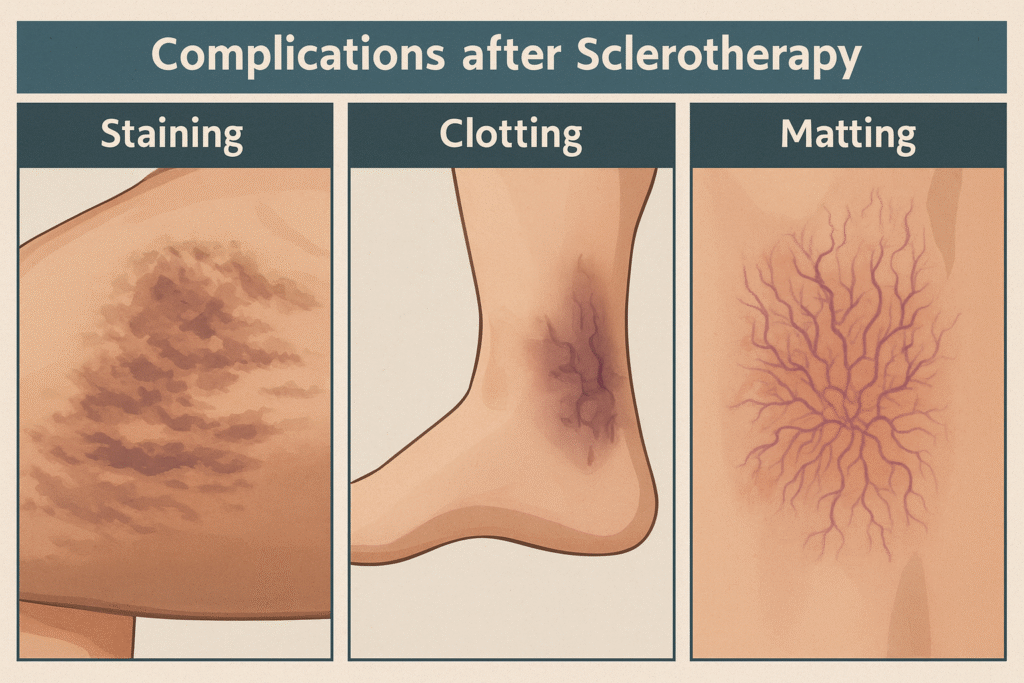
Spider vein procedures are generally safe, but like all medical treatments, they carry some risks. Patients should be aware of:
- Pigmentation (hyperpigmentation): Brownish discoloration along the treated vein. Very common after sclerotherapy, but usually fades over months.
- Matting: Fine red networks of tiny veins that can form after treatment. Often temporary, but many times requires repeat sclerotherapy to over several sessions to resolve. Why this occurs is not clearly defined, but will often resolve spontaneously after several months.
- Clotting: Spider veins feel large, bulky, and appear black after treatment. Occurs if treated vessel was large, inadequate compression was applied, or they are very close to the surface of the skin. Often need evacuations to limit hyperpigmentation.
- Mild burning, stinging, or itching at the injection site (short-lived).
- Bruising or redness for a few days.
- Rare but serious complications (e.g., allergic reactions, skin ulceration, or inadvertent injection into arteries) are very uncommon when performed by experienced specialists.
At VWCLA, we use careful techniques and follow evidence-based safety protocols to minimize risks. Spider vein treatment should be done slowly, spread over many sessions, so that results are excellent with minimal complications. Most patients will have some minor complications and our goal is to walk you through the process so that you will know what to expect and obtain the result you want.
Why Choose Vein & Wound Center of LA for Spider Vein Treatment
• Accurate Diagnosis: We use ultrasound when indicated to determine whether spider veins are fed by deeper venous sources.
• Expert Experience: With thousands of vein procedures performed, Dr. Christopher Kim evaluates both surface clusters and deeper patterns.
• Advanced Treatment Options: We offer sclerotherapy, laser treatments for appropriate cases, and targeted approaches for feeder veins.
• Convenience & Comfort: All treatments are performed in-office using minimally invasive methods with minimal disruption to daily life.
• Patient-Focused Results: Treatment plans reflect your symptoms, circulation patterns, and cosmetic goals.
References
• Society for Vascular Surgery (SVS), American Venous Forum (AVF), American Vein & Lymphatic Society (AVLS). Clinical Practice Guidelines (2023/2024).
• Cochrane Review (2021). Treatment for Telangiectasias and Reticular Veins.
• Lupton JR, Alster TS. Sclerotherapy vs. long-pulsed 1064 nm Nd:YAG.
• Ianosi G et al. Nd:YAG laser for <1 mm telangiectasias.
• Tan MKH et al. Post-sclerotherapy compression systematic review.
• NICE CG168. Varicose veins: diagnosis and management.
• Goldman MP, Weiss RA. Dermatologic Surgery, 2017.
Frequently Asked Questions
Is sclerotherapy effective for spider veins?
Yes. Randomized and controlled studies show sclerotherapy clears telangiectasias and reticular veins more effectively than placebo.
When is laser preferred over sclerotherapy?
Laser treatment is best for very small (<1 mm) spider veins, facial veins, or in patients with needle phobia or sclerosant allergy. It may be a good option as well for people who have large amounts of scattered, diffuse telangectasias. For most leg spider veins, sclerotherapy remains first-line. Sclerotherapy will work the best especially in traditional situations where a reticular or feeding vessel is involved
Do I need an ultrasound before treatment?
If symptoms or patterns suggest reflux, ultrasound helps identify underlying disease.
Should I wear compression after treatment?
Short-term compression may improve cosmetic outcomes and reduce minor side effects. Evidence is mixed, so we tailor it to each patient. Small areas of spider vein treatment may not require full compression garment wear, and local compression only for a few days may be adequate.
How many sessions will I need?
Multiple sessions are common, especially for dense clusters. Temporary pigmentation, bruising, or matting may occur; pigmentation typically fades over time. Serious complications are rare with proper technique. Vein treatments should be considered a process rather than a one-time event.