Varicose Veins in Hollywood, CA
Are you experiencing pain, swelling, or unsightly veins in your legs? You might be dealing with varicose veins, a common condition affecting many individuals in Los Angeles and beyond. Varicose veins are enlarged, twisted veins that often appear blue or dark purple and can cause discomfort or lead to more serious health issues if left untreated.
At the Vein & Wound Center of LA, we specialize in the accurate diagnosis and treatment of varicose veins using advanced duplex ultrasound mapping and minimally invasive procedures. Many vein centers treat varicose veins the same way for every patient, but the reality is more complex: varicose veins can be both a cause and a result of saphenous vein reflux. That’s why correct diagnosis is the first step to long-lasting results.
What are Varicose Veins?
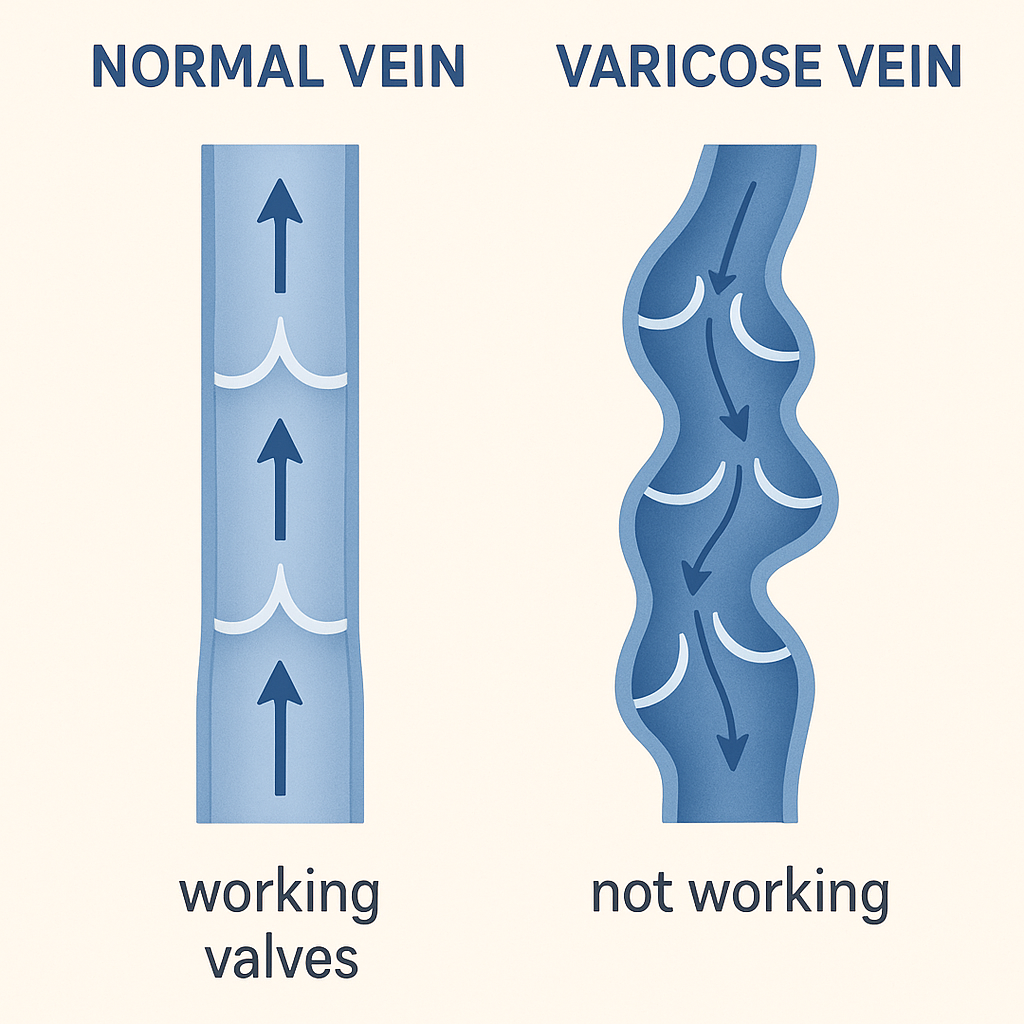
Varicose veins are enlarged, twisted veins that commonly appear on the legs and feet. They develop when the one-way valves inside your veins, which are responsible for keeping blood flowing toward the heart, become weakened or damaged. As a result, blood begins to flow backward and pool in the veins, causing them to stretch, bulge, and become visibly distorted.
While many people associate varicose veins with cosmetic concerns, the condition can lead to a range of physical symptoms. These may include aching, heaviness, burning, swelling, or cramping in the legs—especially after standing or sitting for extended periods. In more advanced cases, varicose veins can contribute to skin discoloration, irritation, or even open sores (venous ulcers) that require medical attention. Early diagnosis and treatment are important to prevent progression and improve comfort and circulation.
What Causes Varicose Veins?
Varicose veins develop due to increased pressure within the veins, often caused by a combination of lifestyle, genetic, and physiological factors. Some of the most common causes and risk factors include:
- Genetic predisposition: A family history of varicose veins significantly raises your risk, as vein valve weakness can be inherited.
- Prolonged standing or sitting: Occupations or daily routines that involve long periods of immobility can hinder proper blood circulation, increasing pressure in the leg veins.
- Obesity: Carrying excess weight puts additional strain on leg veins, making it harder for blood to flow efficiently.
- Pregnancy: Hormonal changes and increased blood volume during pregnancy, along with pressure from the growing uterus, can lead to vein dilation and valve dysfunction.
- Age: As we age, vein walls and valves naturally lose elasticity and strength, making older adults more prone to varicose veins.
- Prior blood clots or trauma: Blood clots can cause damage to venous valves, causing leak points and varicose veins to develop downstream.
Understanding these contributing factors can help you make informed decisions about prevention and when to seek treatment.
Symptoms and Risks
Identifying varicose veins early can prevent complications. Common symptoms include:
- Aching or heavy feeling in the legs
- Burning, throbbing, muscle cramping, and swelling
- Worsened pain after sitting or standing for long periods
- Itching around one or more of your veins
- Skin discoloration around a varicose vein
If left untreated, varicose veins can lead to more severe issues such as ulcers, bleeding, or deep vein thrombosis (DVT).
Treatment Options at Vein and Wound Center of LA
Thanks to advances in vascular medicine, patients no longer need to rely solely on vein stripping or invasive surgery. Today’s varicose vein treatments are minimally invasive and often performed in-office with little downtime. These treatments include:
- Endovenous Laser Therapy (EVLT): EVLT uses laser energy to seal the unhealthy vein, rerouting blood flow to healthier veins. The procedure is performed under local anesthesia and typically takes less than an hour.
- Endovenous Radiofrequency Ablation (RFA): Similar to EVLT, RFA uses radiofrequency energy to heat and close the affected vein. It is effective for larger varicose veins and provides quick symptom relief.
- Sclerotherapy: A medical solution is injected directly into smaller varicose or spider veins so they collapse and fade. It’s ideal for cosmetic improvements and symptom management. We offer visual sclerotherapy and ultrasound-guided sclerotherapy.
- Ambulatory Phlebectomy: This outpatient procedure involves tiny incisions to remove surface varicose veins. Phlebectomy is often used in conjunction with other treatments like EVLT or RFA for comprehensive care.
- VenaSeal™: VenaSeal is a medical adhesive used to close problematic veins without heat or tumescent anesthesia.
- ClariVein®: ClariVein is a mechanochemical treatment that combines a rotating catheter with a medicated solution to seal the vein without heat.
- Varithena®: Varithena is a foam sclerosant used to treat veins that are difficult to address with standard catheter-based techniques.
• Compression Therapy: While not a cure, medical-grade compression stockings improve circulation and reduce symptoms such as pain and swelling. They are often recommended in conjunction with in-office treatment.
Varicose Veins as a Symptom of a Leak Point
Visible varicose veins are rarely the whole story. They usually reflect a deeper “leak point” in the venous system, where faulty valves allow reflux to feed tributary veins. These leak points can be located in:
- The great saphenous vein (GSV)
- The small saphenous vein (SSV)
- Perforator veins
- Tributary (branch) veins
- Pelvic veins
Treating only the visible varicose veins without identifying the source often leads to recurrence.
The Role of Duplex Ultrasound in Vein Mapping
Duplex ultrasound (DUS) is the gold standard for evaluating venous disease. It provides a real-time map of reflux, helping vein specialists determine: The exact origin of venous leak points Whether reflux begins in the GSV, SSV, or tributary veins If reflux is ascending (from varicose tributaries upward) or descending (from the GSV downward) Which veins should be treated for long-term success At VWCLA, every treatment begins with a complete DUS performed by highly trained vascular technologists, ensuring accuracy before any intervention.
Theories of Venous Reflux: Descending vs. Ascending
Traditionally, descending reflux was thought to be the dominant pattern: valve failure begins at the top of the GSV, and reflux extends downward into tributary veins.
Emerging evidence, however, supports the existence of ascending reflux: reflux may originate in tributaries, traveling upward into the saphenous trunk and eventually causing GSV failure.
Recent research has also highlighted the role of nonsaphenous sources of reflux, including perforator veins and pelvic escape points, as well as the contribution of vein wall stress and remodeling to progressive dilation. These factors suggest that varicose vein disease is not always a single-valve problem but a complex interplay of valve dysfunction, venous wall weakness, and hemodynamic forces.
In simpler terms, newer research shows that varicose veins don’t develop the same way in everyone. The problem can begin in the main vein of the leg, in a small side vein, or even in deeper veins connected to the pelvis. These different starting points can push abnormal pressure through the vein network in different directions. This is why some people develop symptoms early, some develop them later, and others have vein maps that look completely different even when their symptoms seem similar. Understanding where reflux begins is essential because treating only the visible veins may not correct the underlying flow problem.
Evidence from Clinical Studies
A key paper by Labropoulos N, Kim H. “Patterns of Saphenous Reflux and Treatment Plan” (Phlebology, 2006) emphasized that treatment must address not just the GSV, but also the tributaries feeding into it, since untreated tributaries can maintain reflux even after ablation.
Similarly, European work (e.g., Whiteley et al.) has described cases of descending versus ascending reflux, sparking debate in the field. While these theories are still under discussion and not universally adopted by societies such as the American Vein & Lymphatic Society (AVLS), they reinforce the principle that careful mapping and individualized planning are essential.
At VWCLA, we integrate this evidence-based perspective into our evaluations. By identifying reflux, whether it arises from the GSV, tributaries, perforators, or nonsaphenous veins, we ensure that the true source of disease is addressed.
These studies highlight why a detailed ultrasound is so important. Some clinics look only at the large veins, but research shows that smaller veins can keep sending blood backward even after the main vein is treated. If these feeder veins are overlooked, symptoms can return. By mapping every vein pathway—including deeper and less obvious ones—Dr. Kim can determine where reflux begins and create a plan that addresses the actual source rather than just the surface appearance.
Why Ablation Isn’t Always the Answer
Endovenous ablation (closing the GSV with heat or glue) is one of the most effective and widely used treatments for venous reflux. However, ablation alone may not address every patient’s problem.
In some people, the reflux actually begins in smaller side veins rather than the main saphenous vein. If only the main vein is treated, those smaller veins can continue pushing blood backward, and symptoms may return. Detailed ultrasound mapping helps identify where reflux starts, so treatment is directed at the right veins, large or small, without performing unnecessary procedures.
At VWCLA, we focus on targeted treatments guided by ultrasound to achieve the best results with the least vascular impact.
Why Choose Vein & Wound Center of LA for Varicose Vein Treatment?
- Accurate Diagnosis: Effective varicose vein care begins with identifying where reflux is coming from. Using detailed ultrasound evaluation, we determine whether symptoms are caused by the saphenous vein, tributaries, perforators, or a combination, so treatment targets the true source of the problem.
- Expert Experience: With thousands of vein procedures performed, Dr. Christopher Kim understands the different patterns of venous reflux and how they appear on imaging. This experience allows us to recommend the most appropriate treatment pathway, including for patients who have been treated elsewhere without meaningful improvement.
- Advanced Treatment Options: We offer minimally invasive procedures such as endovenous thermal ablation, phlebectomy, sclerotherapy, and mechanochemical or adhesive-based treatments to support circulation and long-term leg health.
- Convenience & Comfort: All procedures are performed in-office using local anesthesia. No general anesthesia or stitches are required, and most patients resume normal activities shortly afterward.
- Patient-Focused Results: Your symptoms, goals, and ultrasound findings guide every decision. Whether your priorities involve easing heaviness and swelling, improving skin changes, or treating visible veins, we develop a plan centered around your needs.
Frequently Asked Questions (FAQ)
1. Are varicose veins dangerous?
They are not always dangerous but can worsen over time, leading to swelling, skin damage, or even ulcers if untreated.
2. Do varicose veins go away on their own?
No. Once valves are damaged, veins remain dilated. Only medical treatments can close or remove them.
3. Do varicose veins always mean I need a saphenous ablation?
Not always. Sometimes reflux begins in tributary veins and feeds the saphenous vein. In these cases, treating tributaries may be more effective.
4. What treatments are available?
Minimally invasive options include Endovenous Ablation, phlebectomy, and Sclerotherapy for Spider and Reticular Veins. All are done in-office with minimal downtime.
5. Who should get evaluated?
Anyone with visible varicose veins, leg discomfort, swelling, or skin changes should undergo duplex ultrasound mapping..
6. Can varicose veins cause reflux in the saphenous vein?
Yes. Although reflux often flows downward from the saphenous vein, it can also ascend from varicose tributaries into the GSV.
References
- Eberhardt RT, Raffetto JD. Chronic Venous Insufficiency. Circulation. 2014;130(4):333-346.
- Gloviczki P, Comerota AJ, Dalsing MC, et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines. J Vasc Surg. 2011;53(5S):2S-48S.
- Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005;15(3):175-184.
- Nicolaides AN, Allegra C, Bergan J, et al. Management of chronic venous disorders of the lower limbs: Guidelines according to scientific evidence. Int Angiol. 2008;27(1):1-59.
- Labropoulos N, Kim H. Patterns of Saphenous Reflux and Treatment Plan. Phlebology. 2006;21(1):12–17.
- Whiteley MS, Dos Santos SJ, Harrison CC, Holdstock JM. Descending venous reflux: when the great saphenous vein is refluxing because of varicose tributaries. Phlebology. 2014;29(10):706–713.
- Holdstock JM, Dos Santos SJ, Harrison CC, Whiteley MS. Haemodynamics of varicose veins: effect of stripping the long saphenous vein. Br J Surg. 2014;101(6):709–716.
Take the First Step Toward Healthier Veins in Los Angeles, CA
Don’t let varicose veins disrupt your life any longer. At the Vein and Wound Center of LA, we are committed to helping you regain comfort and confidence. Contact us today to schedule a consultation with Dr. Christopher Kim. Call us at (213) 654-8346, and take the first step towards healthier, pain-free legs.